Service Authorization
Overview
The Department of Medical Assistance Services contracts with Acentra Health (formerly known as Kepro) to handle the service authorization process for Medicaid, Family Access to Medical Insurance Security (FAMIS) and FAMIS Plus clients in the fee-for-service programs. The Acentra Health (Service Authorization) contract excludes:
- Services managed under a separate contract, including pharmacy, dental, transportation, Intellectual Disability & Day Support Waivers, and managed care organization (MCO) vendor services;
- Please contact the Provider Helpline at 1-800-552-8627 (in-state long distance) or (804) 786-6273 (local and out of state customers) for services that are currently authorized by DMAS Medical Support Unit;
- Certain waiver enrollment/service authorizations [pdf] Maintained by DMAS Office of Community Living
- Behavioral Health information can be found on the Behavioral Health webpage.
- ARTS (Addiction & Recovery Treatment Services) information can be found on the Addiction and Recovery Treatment Services webpage.
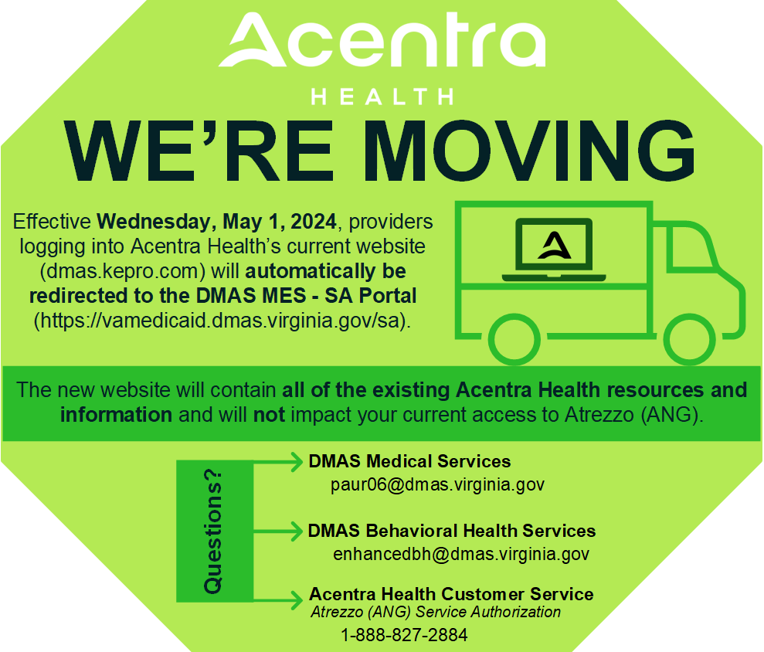
Acentra Health accepts service authorization requests via Atrezzo Next Generation (an interactive web-based application), telephone, paper, and fax submission. The preferred submission method is through direct data entry for a quicker response. Specific information regarding the service authorization requirements and methods of submission may be found on the contractor’s website at https://dmas.kepro.com/.
For service authorization questions, please email paur06@dmas.virginia.gov regarding medical services and enhancedbh@dmas.virginia.gov for behavioral health services.
New Process for Submitting Service Authorizations
The Department of Medical Assistance Services (DMAS) is making significant changes to the process used to submit service authorization requests for Fee-for-Service (FFS) members. Effective November 1, 2023, all providers who provide services to Medicaid and FAMIS members will submit service authorizations to Acentra Health (formerly known as KePro).
This change will affect providers who perform services for the following programs:
- All Behavioral Health and ARTS Services
- Baby Care Program
- Continuous Glucose Monitors
- EPSDT Private Duty Nursing
- EPSDT Private Duty Nursing MCO School Based Carve Out
- Out of State Imaging
- Genetic Testing
Acentra Health is offering a series of specific trainings for administrators, medical providers, behavioral health providers and others to learn about and understand the new process. It is critical that all staff involved in the service authorization request process register for and attend a training session.
For more information, read the Medicaid bulletin dated Sept. 18, 2023 and view the list of upcoming training classes.
Request Submission Options
- Overview of Service Authorization Contractor - Please see the Atrezzo Provider Portal UM User Guide for additional information.
- Atrezzo Connect - Log In;
- U.S. Mail - Acentra Health 6802 Paragon Place, Suite 440, Richmond VA, 23230;
- Telephone - 1-888-VAPAUTH (827-2884) 804-622-8900 (local);
- Fax - 1-877-OKBYFAX (652-9329)
- Expansion requests: https://dmas.kepro.com/
Emergency Medicaid Service Authorization Requirement - Effective March 13, 2023
Effective March 13, 2023, Kepro will begin reviewing inpatient hospital requests for nonresident alien emergency inpatient admissions when the member is in the following aid categories designated for non-resident aliens who require emergency services:
- Aid Category 112 Expansion population/Modified adjusted gross income (MAGI) Adults
- Aid Category 113 Non-MAGI/ABD/Children
Inpatient hospital providers are to submit their request through Kepro's secure portal, Atrezzo, using service type 0400. Kepro will review the request for emergency hospital admissions. Since inpatient hospital requests are only for emergency services for this population, qualifying admissions must be preceded by treatment and transfer from an Emergency Department (ED) with appropriate physician certification for inpatient services.
For admissions prior to July 1, 2022, providers are to reference the Physician/Practitioners Manual and the Hospital Manual, Chapters 4, in both manuals. For admissions on and after July 1, 2022, providers must refer to the Emergency Medicaid Non-Resident Alien Supplement.
Hospital to Hospital Transfers
Documentation for transfers will include initial hospital ED records, inpatient admission certification, and discharge note/transfer summary to support that emergent care is still necessary. Transfers are for treatment that the initial hospital cannot provide, usually a higher level of care.
Grace Period for Providers
From March 13, 2023, through April 30, 2023, Kepro will waive timeliness for the inpatient hospital admission when the aid category is 112 and 113. This grace period will allow admission dates of service from July 1, 2022 – April 30, 2023 to be submitted without timeliness penalty, as long as the case is submitted by April 30, 2023 in Atrezzo. Kepro’s Atrezzo system is available 24/7 for submission of requests.
Refer to the DMAS Medicaid Memo dated March 30, 2023.
Provider Memo Updates
There are service authorization process changes that may impact your services to Acentra Health (formerly known as Kepro). Please use the Medicaid Memo search link for additional information.
Reminder: Service Authorization Expiration Dates
You may have members whose service authorizations will be expiring next month. If the member continues to need the services, you will need to submit a request for services to the Department of Medical Assistance Services designated service authorization contractor prior to the end of the current authorization. THERE ARE NO AUTOMATIC RENEWALS.
For services that are authorized by Acentra Health, the service authorization request may be submitted through direct data entry (DDE), fax, phone or and US mail. The preferred method is by DDE for a quicker response through Acentra Health’s provider portal, Atrezzo Next Generation (ANG). To access ANG on Acentra Health's website, go to https://dmas.kepro.com/.
 Virginia Medicaid
Virginia Medicaid